How medical experts are deciding which treatments should be used for COVID-19: Â鶹ĘÓƵ expert

Published: May 1, 2020
Ontario doctors and scientists have formed two high-powered committees to sift through the and on how best to treat patients with COVID-19.
The two committees – one charged with recommending the most effective drugs and the other with how best to manage critical illness – were formed to ensure treatment for patients hospitalized with the novel coronavirus in Ontario is based on the best science available.
Dr. Andrew Morris, an infectious disease specialist at the University Health Network and Mount Sinai Hospital in Toronto, as well as a professor in the University of Toronto’s Faculty of Medicine, is the chair of the committee focused on providing drug guidance, called the .
This 20-member antimicrobial committee formed in March includes infectious disease specialists, pharmacists, ethicists and even a patient who has recovered from COVID-19. As Morris puts it, he and his colleagues felt, “There was a sense of impending doom and we needed to be prepared to have something to offer people.”
Weighing evidence against emotion
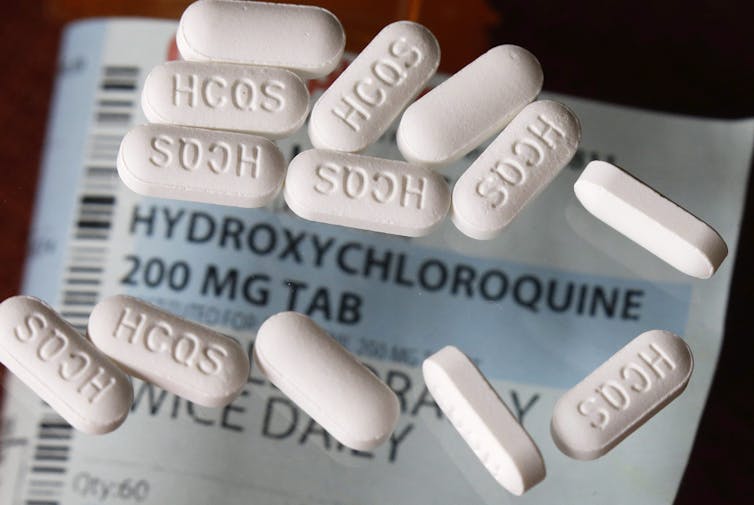
The – some from experts, others from amateurs – underlines the importance of the two committees’ work. For example, medications, such as the despite dangerous side-effects and little evidence of effectiveness against COVID-19.
As a veteran in the treatment of lethal infections, Morris says, “People, if given the chance, will over-treat based on emotion and not on cognition. They will choose emotion nine times out of 10.”
Morris says even the most evidence-based physicians have been swayed by the lure of hydroxychloroquine as a readily available treatment.
“It has turned out to be a total scam,” he says. “It was clear there was no peer review, and no hard data on the benefit.”
The antimicrobial committee recommended overwhelmingly in mid-April against prescribing hydroxychloroquine, even for the sickest patients.
They have tried to be cautious in their recommendations because, as Morris says, “None of are designed specifically to treat COVID-19. The likelihood of a game-changing treatment at this point in time is incredibly small.”
Starting from scratch
There are no national or provincial guidelines for the treatment of most infectious diseases. So, the committee — all volunteers — has worked entirely from scratch to develop its recommendations and disseminate them to health-care providers.
Ontario Health has helped disseminate the committee’s .
The committee has so far not recommended any medications unless a patient is enrolled in an approved clinical trial. One reason, Morris says, is based on his infectious disease expertise and experience with COVID-19: “The human body and nature will actually do a decent job of fighting the infection. Unless we know what we are doing, the worst thing we can do is harm patients with COVID-19.”
Evidence-based critical care
For the sickest patients in intensive care units, a committee of critical care specialists formed the University of Toronto Interdepartmental Division of Critical Care COVID Working Group to provide care guidance. It was formed in March, at the same time as the antimicrobial committee.
This group advises critical care providers in Ontario on the .
Dr. Nava Maham, a critical care specialist at the University Health Network and a member of the committee says, “Our job is to apply evidence-based practice that we know works, provides a benefit to patients and does not harm them.”
Five critical care physicians from Toronto’s largest academic hospitals comprise the committee. These doctors care for Ontario’s sickest COVID-19 patients, even as they update the guidelines twice each week.

Reflecting on her dual responsibilities, Maham says, “[COVID-19] is something we are all consumed by. There are no business hours during this pandemic. We are either taking care of patients with critical illness or desperately trying to keep up with the literature, and keep our guidelines as up-to-date and as helpful as possible.”
Maham and her colleagues on the committee receive daily input from physicians across Ontario and from heavily hit areas, such as Italy.
“I feel that we know as much as anyone anywhere else in the world given the level of collaboration we are seeing,” she says.
The temptation of unproven treatments
Like Morris, Maham is wary of unproven therapies.
“There is a human desire to want to do something,” she says. “There is a feeling that if you are administering a drug, then it feels better than doing nothing.”
However, except for approved clinical trials, she cautions that health-care providers should resist the urge to test therapies on patients.
“Because we know these could come with significant and serious harm,” she says.
She is optimistic the two new committees will prevent harm to Ontario patients.
“People are working around the clock to ensure that we give every patient the best chance to recover, and they can feel comfortable knowing their care will be guided with the best available evidence.”
is an emergency physician and an assistant professor in the department of family and community medicine at the Faculty of Medicine at the .
This article is republished from under a Creative Commons license. Read the .



